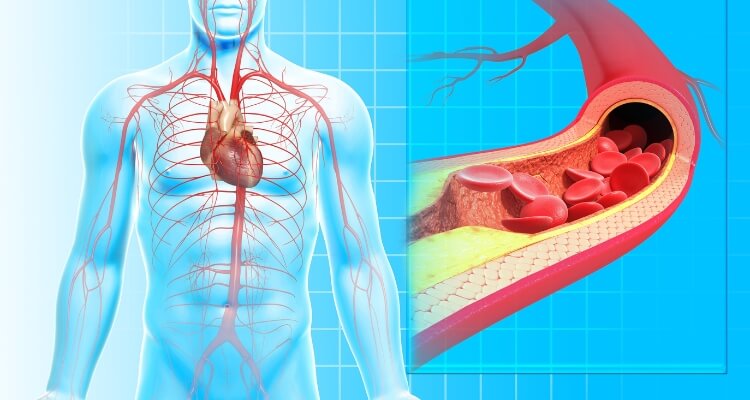
Atherosclerosis, often referred to as a silent disease, slowly narrows and hardens the arteries throughout the body. Although it can silently progress for years, it’s essential to be familiar with the potential symptoms that may present themselves when the disease starts to affect various bodily functions.
Atherosclerotic cardiovascular disease
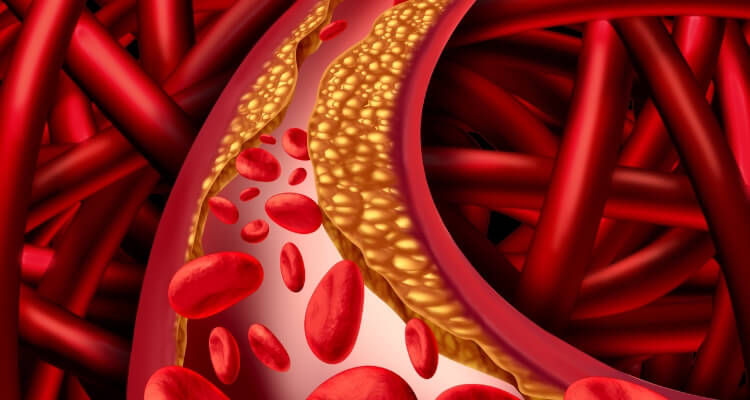
Atherosclerotic cardiovascular disease (ASCVD) is a pervasive condition that involves the buildup of cholesterol plaque in the arteries, leading to a host of health problems. The key manifestations of ASCVD include acute coronary syndrome, peripheral arterial disease, and critical events such as myocardial infarction (heart attack) and stroke. A leading contributor to morbidity and mortality in the United States, ASCVD demands urgent attention and understanding.
Risk Factors of ASCVD:
ASCVD doesn’t develop in a vacuum; it’s the culmination of various lifestyle choices and genetic predispositions. Risk factors include dyslipidemia (abnormally elevated cholesterol or fats in the blood), diabetes mellitus (DM), obesity, an inactive lifestyle, hypertension (high blood pressure), smoking, and family history. These factors are critical to ASCVD risk assessments and help shape the strategies for prevention and treatment.
Symptoms of Atherosclerotic cardiovascular disease
Atherosclerosis often doesn’t cause symptoms until it significantly narrows or entirely blocks an artery. Many people don’t realize they have this disease until they have a heart attack or stroke.
These symptoms vary based on which arteries are affected.
Heart – Coronary Arteries
When atherosclerosis affects the arteries that supply blood to the heart (coronary arteries), symptoms may include:
- Chest pain (angina): This can feel like pressure or tightness in the chest, often triggered by physical activity or stress.
- Shortness of breath: If your heart can’t pump enough blood to meet your body’s needs, you may experience breathlessness.
- Fatigue: You may feel unusually tired, especially during times of physical exertion.
Brain – Carotid Arteries
If atherosclerosis narrows or blocks the arteries leading to the brain (carotid arteries), signs and symptoms may include:
- Sudden weakness in the limbs: You may feel a sudden loss of strength in your arms or legs.
- Difficulty speaking: Speech may become slurred or difficult to understand.
- Facial drooping: One side of your face might droop or become numb.
- Severe headache: Sudden and severe headaches can occur.
- Dizziness or loss of balance: You might feel unsteady or experience an unexplained fall.
- Trouble with vision: You may have sudden blurred or double vision, or sudden loss of vision.
Legs, Arms, and Pelvis – Peripheral Arteries
When the peripheral arteries, which supply blood to your legs, arms, and pelvis, are affected by atherosclerosis, you may experience:
- Painful cramping during activities: You might experience pain or cramping in your legs or hips while walking, climbing stairs, or exercising.
- Numbness or weakness: Your legs or arms may feel numb or weak.
- Coldness: Your legs or feet might feel cold to touch, especially in comparison to the other side.
- Skin changes: You might notice color changes in your legs or feet, and wounds or ulcers may not heal properly.
10-Year ASCVD Risk:
Understanding a patient’s 10-year ASCVD risk is fundamental to establishing appropriate medical management. This risk prediction helps clinicians decide if cholesterol-lowering medication like statins should be introduced and informs other potential lifestyle modifications. The goal is to prevent the long-term complications associated with ASCVD, including heart attack and stroke.
Traditional Lipid Testing:
Traditional lipid tests, which measure markers such as total cholesterol, low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), and triglycerides, play a significant role in evaluating ASCVD risk. These tests are also used for regular screening and monitoring to ensure that medical interventions are working and that risk factors are under control.
Nontraditional Markers:
While traditional markers are invaluable, there’s a growing recognition for nontraditional, novel markers in the evaluation of high-risk patients. Apolipoproteins, lipoprotein particles, and high-sensitivity C-reactive protein (hsCRP) are proving to be effective indicators of cardiovascular risk.
Apolipoproteins are proteins that bind lipids to form lipoproteins, contributing to plaque formation. Lipoprotein particles, especially the small, dense ones, can slip through the arterial lining more easily than larger ones, increasing the chance of plaque development. High-sensitivity C-reactive protein (hsCRP) is a marker of inflammation in the body, and high levels can indicate an increased risk of ASCVD.
Conclusion:
Understanding the intricate layers of ASCVD, from risk factors to lipid testing and potential markers, is the key to managing this widespread disease. As researchers and clinicians continue to explore innovative approaches to diagnosis, treatment, and prevention, the hope for effectively combating ASCVD continues to grow. It is a condition that affects millions, but with continued dedication to understanding and mitigating risk, we can make significant strides in reducing its impact.